Your overall health is important to us, and the university offers a variety of benefits to help support your physical and mental health. University of Louisville offers four health plans through Anthem Blue Cross Blue Shield. Sharp Health Plan continues to be recognized in California and nationally for their high-quality care and service. They are the highest member-rated health plan in California, and they also hold the highest member ratings for health care, personal doctor and specialist among reporting California health plans. As part of Sharp HealthCare's integrated delivery system, Sharp Health Plan directly connects members to an expansive network of nationally recognized doctors, elite-rated medical groups and hospitals.
Who we areAnthem, Inc. is one of the largest health benefits companies in the United States. With local service and the value of the Blue Cross brand, we have been committed to ensuring our members have access to affordable health benefits for over 80 years. In 2004, WellPoint Health Networks Inc and Anthem, Inc. merged and became the nation's leading health benefits company. In December 2014 WellPoint Inc. changed its corporate name to Anthem, Inc. Anthem has about 40 million members and is ranked 33rd on the Fortune 500.
Both plans cover services such as preventive care, doctors' office visits, hospitalization and prescription drugs. However, there are important differences between them—both in your choice of providers and what you pay when you get care (your out-of-pocket costs). WHA offers affordable, quality health care to its neighbors in Marin, Napa, Sacramento, Solano, Sonoma, Yolo and parts of Colusa, El Dorado, Humboldt, and Placer counties.
UnitedHealthcare Signature1 - The Signature plan includes our full network of contracted providers. With this HMO plan, members simply choose a primary care physician from our full network of contracted providers to coordinate all their medical care. They can then visit their PCP for routine checkups, and when they need to see a specialist, their PCP provides a referral. Members are charged only a copayment for each doctor's visit. UnitedHealthcare of California is committed to providing quality coverage and affordable benefits to help keep you and your family healthy.
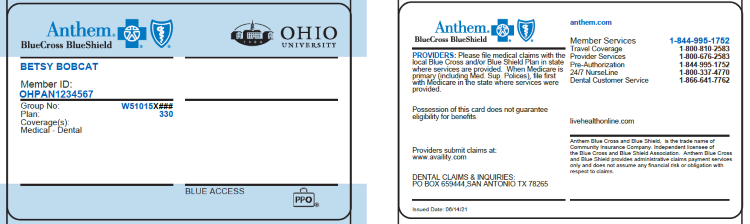
Our plans offer more than just doctor visits; preventive care services are also provided for every member of the family. Anthem Blue Cross HMO. You choose a primary care physician —from a UC Medical Center or the Anthem Blue Cross HMO network—who coordinates all your care, including behavioral health. Except for emergencies, only care received from UCMC or Anthem HMO doctors and at HMO facilities is covered at the in-network level.There's no deductible. For most services, you pay a small copayment and the plan pays the rest. This plan combines traditional medical coverage with a Health Savings Account .
Under this plan, all covered services (except preventive services/prescriptions) are subject to the annual deductible. The deductible is a dollar amount of out-of-pocket costs you must pay each year before the plan will begin paying its share of your healthcare expenses. The nice thing about this plan is that you can pay for that deductible using the tax-free funds in your HSA. Once the deductible has been met, most in-network services are covered with a 20% coinsurance. Our Signature plan offers access to a full network of contracted providers with more than 62,590 physicians and health care professionals, and 273 hospitals.
The Advantage, Alliance and Harmony plans offer the same level of benefit coverage as our Signature plan but has a narrower network of contracted providers. You can find listings for physicians and hospitals in our provider directories. With a mix of benefits that deliver patient-centered care, health and wellness programs and award-winning customer service, UnitedHealthcare is a smart choice for your family's health care coverage needs.
Because of its large network of providers, giving you many choices for where you get medical services. Anthem has a variety of health insurance plans available including options for individuals, families, Medicare, Medicaid and group insurance. Beginning in 2013, Anthem Blue Cross became the behavioral health provider for Anthem HMO and PPO plans. If you are enrolled in one of these Anthem plans, you do not need a referral from your primary care physician in order to receive mental health services. Visit Anthem's website at /ca for a list of behavioral health providers.
WHA is all about helping people obtain quality health care. We also support medical innovation and promote whole-person health to suit the various needs of the communities we serve. WHA offers affordable coverage to employer groups, individuals and families, and Medicare retirees for every stage of life. We are here to help you stay healthy and facilitate the care you need when you need it. What began 70 years ago as an innovative health care program for shipyard and steel mill workers has become the model for health care in the 21st century. Serving 11.8 million members in 8 states and the District of Columbia, Kaiser Permanente is the convenient, affordable health plan you can rely on to keep your employees and their families healthy and engaged.
From preventive care that catches health problems early to specialty care for illnesses and injuries, we've got your employees covered. Health Net Decision Power Healthy Discounts is not intended as a benefit program purchased from Health Net. The Decision Power Healthy Discounts program is made available to specified Health Net members free of charge. Decision Power Healthy Discounts programs offer discounts on products/reduced-fee services. However, the products and services available from Decision Power Healthy Discounts are not part of your medical benefits plan, but are part of Health Net's Wellness Program available to its members. Decision Power Healthy Discounts providers are independent businesses.
Services and/or supplies must be purchased directly from a Decision Power Healthy Discounts provider. PPO members have the option to see out-of-network providers. If you're enrolled in family coverage, you must meet the family out-of-pocket maximum before Anthem will pay 100% of expenses. The health care network specified by your Anthem insurance policy will determine whether you have access to in-network providers in other states. When submitting an out-of-state claim, you must contact Anthem's customer service department because the process may be different. With Sutter Health Plus, members gain access to an integrated network of high-quality healthcare providers, including many of Sutter Health's hospitals, doctors and healthcare services.
The MetLife DHMO plans provide access to a large network of dental providers throughout California. Preventive dental care is an important part of overall health and MetLife is committed to ensuring that its members receive a high level of dental care. As part of this commitment, all Quality Management Activities are designed to meet or exceed NCQA standards. These standards are applied to plan design, through the credentialing of network providers, member services standards and on-going peer review and facility audits. When you elect the Anthem PPO HDHP, you are also eligible to elect a Health Savings Account , a special tax-advantaged bank account to help cover your out-of-pocket healthcare costs.
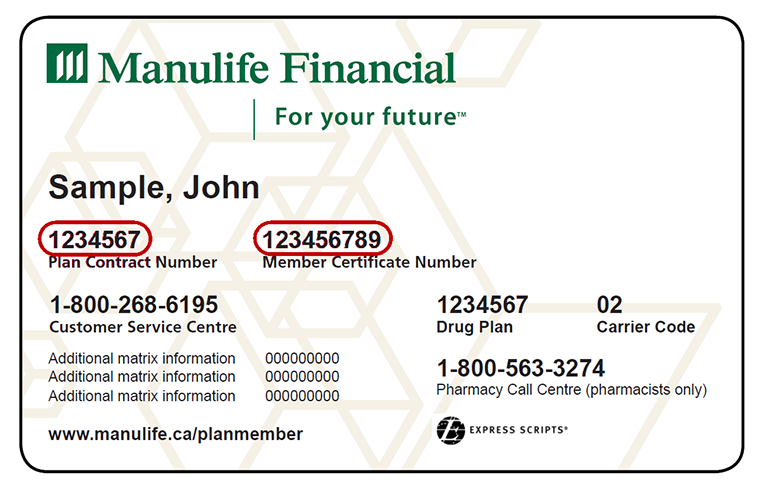
If you forget or aren't sure what type of health insurance plan you have , you can find out on your BCBS ID card. If you have an HMO, your card may also list the physician or group you've selected for primary care. Determining whether a provider is in-network is an important part of choosing a primary care physician. UnitedHealthcare Alliance1 - Designed with affordability and quality in mind, the Alliance plan puts members at the center of a "patient-centered care" experience to promote better outcomes and lower costs.
Alliance physicians are committed to using and sharing de-identified health data to advance best practices and help deliver better care, every step of the way. UnitedHealthcare Advantage1 - The Advantage plan offers the same level of benefit coverage as a traditional HMO plan at a lower premium. The Advantage plan offers a narrower network of contracted providers.
Members must choose a PCP from the Advantage network to coordinate all their medical care. It's best to check your health care options before using the emergency room . Plus, when you visit in-network providers, you may pay less for care. Blue Cross Blue Shield offers employer-provided health insurance or group health insurance.
The deductible is the amount you must pay out-of-pocket before the plan will begin to pay benefits. The deductible applies to all covered services except preventive services/prescriptions. When one or more family members are covered, the family deductible must be met before services are covered for any member. Anthem offers different types of health insurance, and plan types include HMO, PPO, EPO, prescription drug plans, vision, dental, short-term insurance and supplemental insurance. Seniors can sign up for Medicare plans, and those with low incomes can get Medicaid plans administered by Anthem. Anthem's size has advantages such as being widely recognized and having the financial weight to provide members with good tech tools and helpful medical resources.
There are also downsides including poor customer service and a lack of personalization. Blue Cross Blue Shield members have access to medical assistance services, doctors and hospitals in most countries around the world. To learn more about your international coverage visit BCBS Global® Core or contact your local BCBS company. VSP is dedicated to offering affordable, high-quality eye care plans that promote visual wellness and improve their member's quality of life. As the nation's largest provider of eye care coverage, thousands of companies rely on VSP to provide a range of vision plans. Cigna + Oscar is designed to work for small businesses like yours.
We're here to provide affordable care that works for your team, and insurance that cares for your business. Benefits elections must be made within 30 days of your start date or qualifying event. However, for any eligible dependent you elected to cover, you must submit documentation within 60 days of your benefits effective date to verify your dependent's eligibility.
Verifying eligibility helps UofL to ensure compliance with the health plan provision, and manage the increasing costs of health care. Submit copies to the Human Resources office at 1980 Arthur Street. The policies are usually popular in states where they're available, and the company has a large network of medical providers. Keep in mind that Anthem has a reputation for denying claims, and you may be able to avoid problems by carefully reviewing plan documents or contacting the insurance company before receiving care. There are many plans to choose from, and members have access to useful resources and digital tools.
Plus, monthly rates are usually a good value, and the company has a large network of providers. However, the company has a poor reputation for customer service, has repeatedly been fined for violating customer grievance practices, and has a high rate of claim denials. You choose the plan that is best for you and your family. Option 1 is the Traditional PPO and option 2, the High Deductible Health Plan with a Health Savings Account.
Health Net ranks the highest in customer service among Health Insurers in Forrester's proprietary 2021 US Customer Experience Index (CX Index™) survey. The ranking was based on responses from more than 85,000 US survey respondents from 13 US industries, including health care plans. EyeMed Vision Care is a leading vision benefits company providing vision wellness programs to more than 140 million members. Members have the choice of thousands of private practitioners and leading optical retailers including LensCrafters® , Sears Optical® , JCPenney Optical® and most Pearle Vision® locations. EyeMed's unique approach to vision care offers substantial savings on eye care and eyewear purchases. We offer enhanced online services for employees and dentists, with quick access to dental benefits and coverage information.
Outpatient therapy is covered the same as a doctor's office visit. When you get care from UC Medical Center or Anthem providers, once you meet your deductible, the plan pays most of the cost and you pay a portion . Participating providers in the HealthKeepers network accept a set free as payment for covered services, keeping costs low. The rate you pay for insurance will vary based on your personal details, where you live and the level of coverage you select. In 2022, individual health insurance plans are likely to be priced slightly higher, and the rate of increase varies by state. WithGinger, you have behavioral coaches, self-care resources, and video-based therapy and psychiatry services at your fingertips.
Plus you can get unlimited text-based support from behavioral health coaches anytime, anywhere through the Ginger app. If you use a network doctor or hospital, your claims will be submitted by that provider. If you see an out-of-network provider, you need to submit the claim yourself.
You must submit a completed claim form or alternative documentation via fax or mailing address. As an alternative to sending a claim form, supply a description of services, a bill of charges from the provider and any medical documents you received from your provider. Your online account is a powerful tool for managing every aspect of your health insurance plan. Whether you need to check on a claim, pay a bill, or talk to a representative, you can easily access all your member features.
We offer affordable health, dental, and vision coverage to fit your budget. Plus, you may qualify for financial help to lower your health coverage costs. Indiana University is an equal employment and affirmative action employer and a provider of ADA services. All qualified applicants will receive consideration for employment based on individual qualifications. Department of Education Office for Civil Rights or the university Title IX Coordinator.
See Indiana University's Notice of Non-Discrimination here which includes contact information. Vision and vision wear coverage is provided through Anthem Blue View Vision. This coverage is included with your medical plan enrollment, but vision services have their own schedule of benefits and network separate from medical benefits.
Blue365® offers our members access to exclusive discounts on health and wellness products and services. Keep it in a safe, easily accessible place like your wallet. Your card contains key information about your health insurance coverage that is required when you need care or pick up a prescription at the pharmacy. Keeping your card in a secure location will also help protect you from medical identity theft.
Quality Care That's Right for YouWhether you need a routine check-up or a specialty procedure, you want the best care you can find. BCBS recognizes doctors and hospitals for their expertise and exceptional quality in delivering care. Learn more about our Total Care and Blue Distinction® Specialty Care designation programs and find a designated doctor or hospital that meets your needs. We offer access to a wide range of doctors, specialists, and hospitals to help you find care wherever you live or work. Our PPO, HMO, dental, and vision networks are among the largest in California.
For 24 years and counting, we've been a reliable partner in your community. We are known for acting with integrity and for interacting honestly with our partners, while building a relationship of trust. We support the doctor-patient relationship and offer access to quality doctors and hospitals.
At Health Net, we believe every person deserves a safety net for their health, regardless of age, income, employment status or current state of health. Founded in California more than 40 years ago, we're dedicated to transforming the health of our community, one person at a time. Today, Health Net's 2,600 employees and 85,000 network providers serve 3 million members. Innovative group product marketing, customer service at the highest level and top-notch administrative expertise at reasonable costs are the familiar characteristics of Assurity's Group Insurance Division. As the first carrier to offer an accelerated death benefit on a group life plan and a group critical illness product, we continue to be among the industry leaders in inventive product design.




















No comments:
Post a Comment
Note: Only a member of this blog may post a comment.